Taking Charge of Your Pelvic Health

Jan 24 2022
Written by Dr Jackie Crowell
Many women admit they don’t know enough about their pelvic health. They even bring their voice down to say “vagina”. I hear countless stories of women who say they have to take time off work because of their pelvic pain and have done so for years. It’s not that they think this is “normal” but have often been dismissed by providers who may not have the answers to the complex puzzle that is pelvic pain.
I am honored when someone walks in my door seeking help with their pelvic health. Not just the first visit but each visit I get to support them in their recovery, I don’t take lightly. After delivering my second baby I suffered from severe pelvic pain. I was in a dark place, despite holding my newborn and having a toddler who adored me. My husband was outstandingly understanding and supportive. Despite his support, I was unable to care for myself, nor those who were my responsibility. I was unable to return to my job as a pelvic floor physical therapist following my maternity leave and I felt like a failure. In hindsight, my seven-month journey didn’t take that long but it felt like an eternity. It was a difficult path but one that has allowed me to be massively empathetic to my patients today. I was a pelvic floor physical therapist before my pelvic pain began and felt fortunate to have the knowledge and resources to fully recover. If you are suffering from pelvic pain, know that there are many options for help.
The purpose of this article is to help arm you with more knowledge. Knowledge is the key to optimal pelvis wellness. In this article, we will explore the pelvic floor to gain a better understanding of what can be done about pelvic pain.
First, what is “Pelvic Health”?
Pelvic health is a broad term that encompasses reproductive, sexual, bowel and bladder function as well as the health of the muscles and joints of the pelvic region. There are numerous factors that impact one’s pelvic area including body weight, posture, activity level, hormonal balance, digestive and mental health just to name a few. I am a pelvic floor physical therapist and while my specialty is the muscles, joints and nerves of the pelvic region, I help my patients work through ‘all the things’ including diet and mental health. Each person is different and finding the right team will be crucial if you’ve had pelvic pain for a prolonged period.
Next, let’s look in the mirror…
Picture by Nydia Blas Boyd @neeksiebeeks
The external genitalia of a female at birth is called the vulva while the canal inside is the vagina. The vulva includes the labia, head of the clitoris and vestibule which is the opening to the vagina. How often have we heard the whole thing referred to as the vagina? This is not our fault. We are a product of generations before us who did not know any better. It’s like calling your face your throat! Consider yourself more “cliterate”. By the age of four, my daughter called her anatomy “VV” for vulva and vagina. When it comes to hygiene, she will tell you slathering soap on her vulva is a no-no.
Why don’t I need soap? The vagina cleans itself and requires an acidic environment to fight off bad bacteria. When harsh soaps are used, the good bacteria is washed away and cannot fight the bad bacteria and thus the pH balance is disrupted. So what? pH disruption can lead to yeast infection, itchy tissues, excessive discharge and bacterial vaginosis.
How do we clean things up if we can’t use soap, you ask? With a ph balanced soap, I recommend washing the anus and the groin area and use only water on the inside of the labia. Scrubbing with a washcloth or loofah is unnecessary. Good Clean Love© makes a soap that is safe even if used on the vulva. Many soaps that are targeted at washing the vulvar region are marketed to make you think you stink, these are red flags. The other ways to get a yeast or bacterial infection is douching. This would only be advised if your doctor tells you to do so or you have had gender affirming surgery.
Now that we have the verbiage and hygiene topic settled, let’s discuss the “pelvic floor.”
The muscles of the pelvic floor are part of the “core.” The core is a canister that includes the diaphragm (top), abdominals (front and sides), lower back (back, duh) muscles and the pelvic floor (bottom).
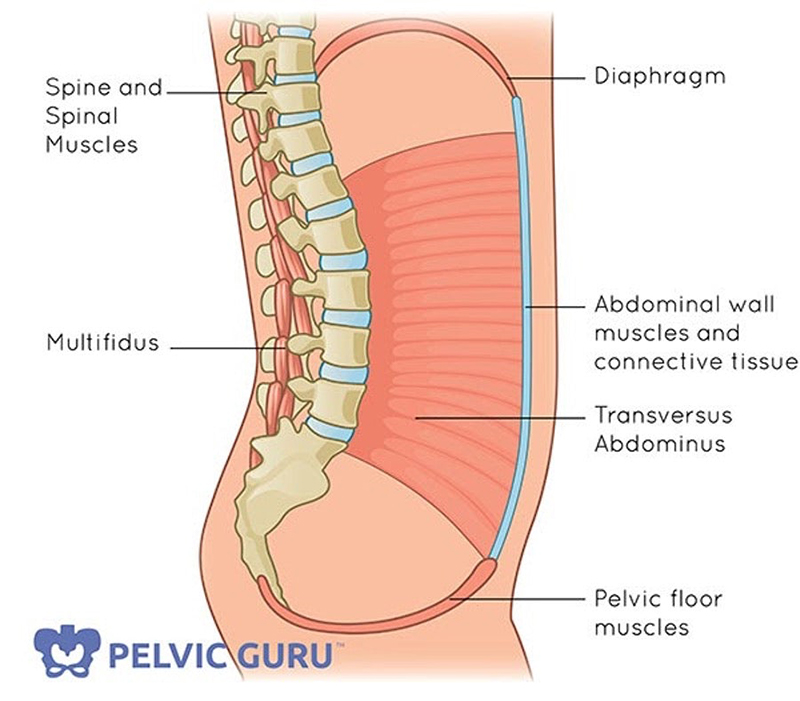
We can find the muscles internally by breathing. Your pelvic floor and diaphragm are intimately connected. Let’s take a deep breath. With each inhale, the diaphragm descends and places a downward pressure of the abdominal contents onto the pelvic floor. The pelvic floor should lengthen and stretch upon inhale and gently lift with each exhale. Tuning into this subtle movement connects mind and body. Feel it? It takes time so not to worry if you don’t feel it yet.
If we hold our breath frequently or breathe shallowly, the pelvic floor can become rigid. When the pelvic floor muscles cannot relax or contract properly our bowel, bladder and sexual function can become impaired. Sometimes this presents as peeing frequently and or constipation. This usually progresses slowly over time. We know that stress can trigger a whole mountain of problems and this is just another one.
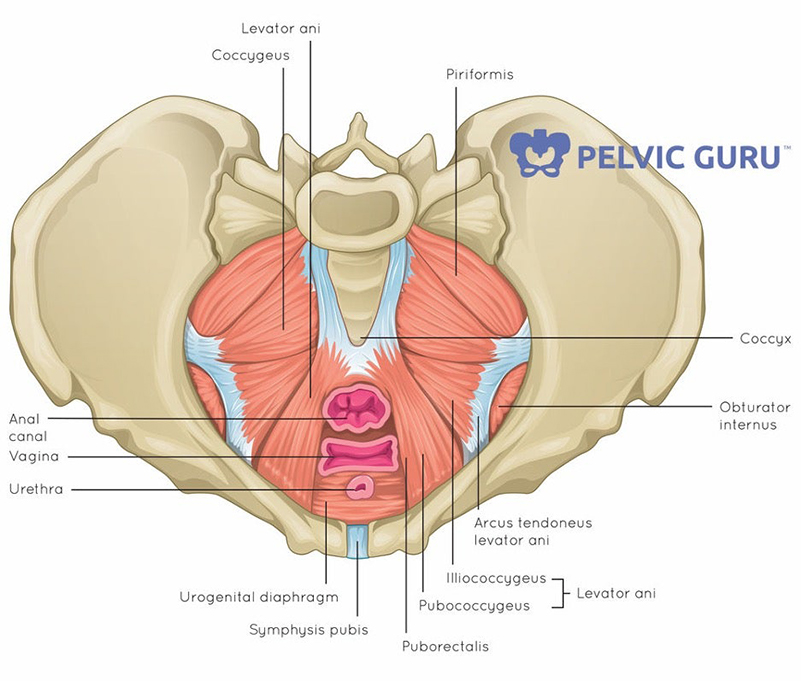
Did you know the pelvic floor for both men and women consists of more than 20 muscles. Here’s a view from the inside (female):
And a view from the outside:
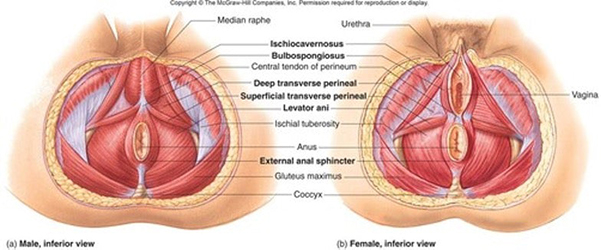
Now that you know more than you may want to about what these muscles look like, lets check into what the muscles of the pelvic floor (PF) do. We’ll start with the superficial muscles of the PF and their role in sexual health.
During arousal, the PCG or pubococcygeus, bulbocavernosus and ischiocavernosus (see muscles above) contract and assist in containing blood in the erectile tissue. In men, this means the penis will become erect and in women the labial tissue and clitoris will engorge. During orgasm these muscles rhythmically contract every 0.8 seconds with climax for 15-51 seconds. If yours last more than 30 seconds consider yourself quite athletic!
The clitoris is shaped like a wishbone. The majority of the clitoral tissue is hidden. The glans (head) of the clitoris has twice as many nerve endings as the glans of the penis, with eight thousand nerve endings! Here’s a 3D model made by Odile Fillod.

Arguably more important than an orgasm is the support the pelvic floor provides.
The pelvic floor supports not only the bladder, uterus and rectum but all the contents that sit in the abdomen beneath the diaphragm. The sphincters are muscles that hold back pee and poo and are part of the pelvic floor too! The bladder itself is also a muscle and like the stomach can become smaller if not stretched. Normal duration between peeing is about 3-4 hours. If you pee every hour or every other hour, you might have a pelvic floor problem. If you have difficulty controlling your bladder or bowel a pelvic floor physical therapist can help.
The next step to an empowered pelvis is early intervention. Most men I see tend to have symptoms for mere weeks by the time they come to see me. Specifically, if their ability to have sexual activity is impaired, they are seeing a urologist right away. For women this isn’t the case as so often their pain has been dismissed, not only by themselves but by providers and closest family members as well.
~Pain with sex? “Use more lube.”
~Painful periods? “That’s sooo normal”
~Pee when laughing? “Me too, that’s so funny.”
What do I do if I have pelvic pain?
First, know you are not the only one and there are so many resources to help. Pelvic floor physical therapy is a holistic and conservative place to start. The majority of states allow “direct access” meaning you can go to any physical therapist without a referral. If you would like to do some research on your own there are several books that help with understanding this treatment.
Heal Pelvic Pain by Amy Stein
Beating Endo by Iris Orbuch and Amy Stein
Pelvic Pain Explained by Stephanie Prendergast and Elizabeth Akincilar
But what can I do right now to help get me started?
- Eat food that makes you feel better, usually this means foods without added sugar, preservatives and is not genetically modified. If your body doesn’t feel better after you eat, you may want to consider eliminating the offending food or beverage.
- Be active. Even a 15-minute walk assists to get blood flowing in the pelvic floor musculature.
- Breathe! I admit this sounds insignificant and one point you could potentially ignore but it might be the most important piece to the puzzle. If you find yourself holding your breath at times or breathing shallowly this is no doubt contributing to the problem.
- Take opportunities to squat all the way to the floor getting your bottom down to your ankles. You don’t have to spend a lot of time here, just get in several daily and you will be doing yourself a favor. Other cultures do this well and don’t suffer from hemorrhoids, constipation and lower back problems like we do in the US.
- Take a bath. This heats up the tissues in the pelvis and relaxes them. (This will not benefit in cases of prolapse where the tissues are loose and need to be strengthened.)
- Avoid Kegels. Often with pelvic pain the muscles are too tight and doing contractions is only going to make it worse.
- Go see a pelvic floor physical therapist. Even if you are not having issues with pain, incontinence or prolapse, a PT can evaluate your lower back, hips and alignment and let you know how you can prevent pelvic floor dysfunction in the future. Your future self will be glad you did.
I have seen patients benefit from changes in diet, meditation, counseling, art therapy, yoga, dry needling, trigger point injections, medications and various procedures as well.
Find a pelvic floor physical therapist in your area: www.pelvicrehab.com
2021. Be the Change.
Early intervention means early success when it comes to pelvic pain. My hope is to never again see a woman walk into my office after having 20 surgeries over the years and say they have not tried counseling, physical therapy or seen a nutritionist. Endometriosis is a condition that on average gets diagnosed nearly a decade after the start of symptoms. Did you know, symptoms of endo can present years before a girl has had her first period as estrogen begins to increase at the start of breast development?
Pelvic pain is not “normal” and no woman should be told there is nothing to do about it.
Understanding your anatomy is a great first step to taking charge of your own pelvic health. I love Semaine’s mission of encouraging women to take charge of their pelvic health and be their own best advocate. We, like all in the field of pelvic health, share a vision that women will no longer accept pelvic pain as “normal.” If you or someone you love suffer from pelvic pain, seek help. Gynecologists are crucial first responders to pelvic pain but pathways to relief can also be found through physical therapy, acupuncture, exercise and counseling. Make sure you feel heard and given options other than medication.
Dr. Jackie Crowell is a licensed doctor of physical therapy specializing in pelvic pain. She is owner of Progressive Pelvis Physical Therapy based in metro Atlanta. She is passionate about pelvic health education and ensuring her patient's achieve a greater quality of life. She is offering Semaine readers a free phone consultation and 10% off their first session. If you would like to know more about how pelvic floor physical therapy can help you, visit her website and register http://progressivepelvis.com/ "here"{ hyperlink}
